Hemangiomas
Hemangiomas

Definition
Hemangiomas are vascular lesions that are not usually present at birth; proliferate during the first years of life and then involute.
A hemangioma is a benign vascular tumor exhibiting unique characteristics in terms of its clinical course and natural history. In early stages, it is composed of endothelial cells. The cells proliferate and make numerous newly formed vessels rapidly. The process of cell proliferation and vessel formation continues throughout the first year of the patient’s life. This is the period that an enlargement of the lesion is evident.
By the end of the first year, the growth phase is completed and then the involution phase begins. This is a much longer process. Eventually the affected area will be completely restructured and all the previously formed vessels will be transformed to fibro fatty tissue. This period is marked by a significant reduction of the lesion’s size.
Hemangiomas are the most common birthmark of infancy. They are benign (not a cancer) stem cell tumors with no genetic or causative factor. Hemangiomas occur in infants only; they never develop in adults.
While not well understood, hemangiomas affect girls three to five times more often than boys. Other associated risk factors include prematurity, low birth weight, and twin pregnancy. While hemangiomas can appear anywhere on the body, more than 80% involve the head and neck, including areas around the mouth, eyes, tip of the nose and cheek.
Recent evidence suggests that hemangiomas are stem cell tumors. They are however benign in their behavior. They grow for a period of time and do not spread to other tissues. Most are quite small and innocuous but some can be quite large. At present, there are no known statistics as to what percentage will be problematic.
Signs and symptoms
At birth
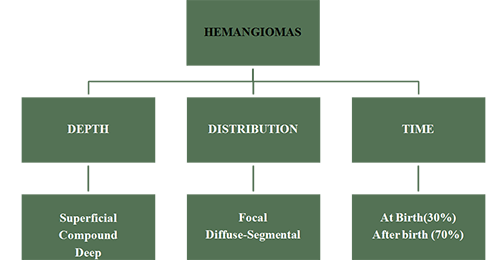
1. 30% of the hemangiomas may be visible at birth
2. 70 % are not present at birth.
First weeks of life
1. A blanched macule may be the first sign of an impending hemangioma. In many cases this macule is unnoticed.
2. Some new vessels begin to form within the affected area, which is now surrounded by a halo.
3. After the first few weeks a rapid development is usually evident. The lesion is raised, and the color is bright red. The clinical appearance may change rapidly. The lesion may be tender to palpation and the child may feel pain if the growth rate is high. During this primary growth cycle the initial clinical manifestations of the lesion's characteristics are present.
In general there are two types of hemangiomas:
Focal Hemangiomas: These are the most common and grow as solitary tumors. They typically grow rapidly in the first few weeks of life and then the growth rate slows. Most of the growth is done by the age of 6 – 7 months. Focal hemangiomas grow in specific sites, known as sites of predilection. They are commonly found in skin or just beneath it. They can also grow in the parotid salivary gland or the breast bud. Focal hemangiomas can be entirely superficial, in which case they are a reddish color, deep in which case the lesion is a bluish color, or compound, with both superficial and deep components.
Segmental Hemangiomas: As their name implies, segmental hemangiomas grow to involve one or more segments of the face and body. This relates to the development of the fetus which takes place segmentally. Their involvement is thus more widespread. Segmental hemangiomas behave differently in that their growth pattern differs. They also grow rapidly in the first few weeks of life, but they can continue to grow for much longer periods of time.
It is not unusual for a segmental hemangioma to grow for up to 2 years. These hemangiomas ulcerate more frequently and can be locally more destructive.
In about 30% of cases, there are other associated developmental abnormalities. These are collectively known as PHACES syndrome. Each of the letters in this syndrome stands for a developmental abnormality. It is important to note that it is uncommon for all of these abnormalities to be present in any one child. Most children with this syndrome will have 2 or 3 of these abnormalities. It is however imperative that all children with a segmental hemangioma be investigated for PHACES syndrome. Up to 30% of children with segmental hemangiomas may have PHACES syndrome.
PHACES syndrome is an acronym:
P. Posterior fossa abnormalities
H. Hemangiomas
A. Arterial abnormalities
C. Cardiac abnormalities
E. Eye abnormalities
S. Sternal defect and or supraumbilical raphe
The majority of Hemangiomas are present in or just to the skin.
There are three clinical manifestations of Hemangiomas according to the depth of the skin layer that they involve.
Superficial Hemangiomas are flat and appear reddish in color as a macular or papular mass or a cluster of small vessels. The skin layer involved is the papillary dermis.
Deep Hemangiomas appear bluish in color and expand the overlying skin. They may also be colorless. The skin layer involved is the reticular dermis. The overlying skin layer may be intact.
Compound Hemangiomas usually have clinical elements of both a superficial and a deep hemangioma. The skin layers involved are the papillary and reticular dermis.
4-6 months
In some babies another growth phase is commonly seen. The vascular mass may continue growing at a fastest rate comparing to its development during the previous month. The baby may feel uncomfortable due to the tissue distension caused by the lesion. This period of the secondary growth cycle may last for one –two months and then the rate of expansion may be reduced.
9-12 months
The growth phase ceases and the transition from proliferation to involution begins. The lesion will soften and shrink from its center to its periphery. The color changes from bright red to a darker, purplish appearance.
1-12 years
In the majority of Hemangiomas the involution commences. The lesion will definitely stop growing and the first signs of the lesion's shrinkage are evident. The rate of involution is variable; so is the point that the involution is completed.
In 60% of Hemangiomas the involution will be completed by the age of 6 years (rapid regression). Unfortunately this fact is not always synonymous to a complete disappearance of the lesion. Atrophy of the skin, residual telangiectasia and previous ulceration markings may still be evident. It has been estimated that 40% of these children will require some form of corrective intervention.
The remaining 40% of Hemangiomas will shrink by the age of 12 (slow regression). In these cases only 20% will disappear completely. The majority, up to 80%, will require an aesthetic correction as residual elements of the lesion are evident.
All hemangiomas involute. Involution simply means shrink. This process may or may not result in a satisfactory outcome. It is important to realize that involution may take many years and the process may be completed in many cases, by 10 to 12 years of age. If it is likely that the outcome of involution will not leave a satisfactory result or if the process is taking too long, then surgery can be considered. It is always preferable to have the child looking as normal as possible by two and half to three years of age. Early surgery has the advantage of healing with less scarring and this should always be taken into consideration.
At the end of involution, one or more of the following may be left over:
Atrophic scar. This is most frequent. Normal skin, especially that of a young child, has an abundance of collagen and elastin in the dermis. This is what makes a child's skin thick and supple, as compared with that of a mature adult. During the process of aging, we lose some collagen as well as elastin and this is in part, what is responsible for the ageing process of skin. A superficial hemangioma that involves skin, will replace the dermis where the collagen and elastin is contained. As the hemangioma involutes, this layer is not replaced and the end result is thin "aged" or atrophic skin. Often, some of the dilated blood vessels will remain and these will be evident as telangiectasia (broken capillaries).
Residual mass. About half of all focal hemangiomas will leave a residual mass of what is known as fibro-fatty tissue behind at the end of involution. This usually takes the form of a soft doughy mass. If the overlying skin was involved, residual telangiectasia (broken capillaries) and atrophic scarring may be left behind.
Hypertrophic scar. Whenever a hemangioma has ulcerated, it always will leave a residual scar behind. This will either be an atrophic (thin) scar or a hypertrophic (thick scar). It will almost never leave normal skin behind.
Indications for treatment
The most common indications for treatment for patients with a hemangioma.
1. The tumor causes marked disfigurement-poor aesthetics
2. Ulceration-Epidermal atrophy
3. Airway obstruction
4. Auditory Obstruction
5. Visual Obstruction
6. Hemorrhage
7. Psychological sequelae
8. Skeletal distortion
9. High output cardiac failure
For explanation of these conditions please see the "risks and complications" section
Risks and complications
1. Ulceration-Epidermal atrophy
Ulceration refers to a loss of skin covering the hemangioma. The cause for this is not known. Ulceration can occur in both focal and segmental hemangiomas. In general, ulceration is extremely painful and the degree of pain seems to be out of proportion to the degree of ulceration. Ulceration usually persists for many weeks or even months.
An ulcerated hemangioma can bleed and at times these bleeds can be severe. Surgery can be used to remove a focal hemangioma and this will dramatically reduce the degree of pain experienced by the child. Hemangiomas that have ulcerated almost always leave a scar and this can be surgically corrected. Hemangiomas of the nose almost always require surgical intervention. Hemangiomas of the upper or lower lip will often require surgical correction.
2. Auditory Obstruction
Hemangiomas may obstruct the external auditory canal and cause a conductive hearing loss. If a lesion is present in or around the canal, the accumulation of debris may result in keratosis obturans
3. Airway obstruction
A hemangioma can also involve the airway and this can lead to obstruction of the child's airway. This can occur in the presence of a beard distribution segmental hemangioma or with a focal hemangioma. The early sign of this is noisy breathing. If this is suspected, the child should be seen by a specialist in this field. We usually recommend an Ear Nose and Throat Surgeon. In some cases, surgery may be necessary to overcome the obstruction.
4. Visual Obstruction
Hemangiomas of the eyelid are serious enough to warrant special consideration. The cornea of the eye is partly responsible for focusing an image on the retina of a child's eye.
The presence of a hemangioma on one or other of the eyelids can interfere with this. As the hemangioma expands, it can deform the cornea by virtue of its weight. This will cause an image to be focused on multiple plains and the result is an out of focus image. This is known as astigmatism. Astigmatism in both eyes is usually not a problem, but if it affects only one eye, the child's developing brain will ignore the out of focus eye and a "lazy" eye will develop. This can result in blindness of that eye.
Periorbital Hemangiomas may interfere with the visual axis and partially block the vision.This also can result in deprivation amblyopia. It is therefore imperative that the child be seen by a pediatric ophthalmologist.
These hemangiomas can be successfully removed and if this is done early enough the astigmatism will reverse. Both Propranolol and steroid injections have also been used to treat these hemangiomas, but, in our experience, surgical resection can completely eliminate the hemangioma as well as the astigmatism (if done early).
5. Hemorrhage
Potential bleeding is one of the parents concern regarding hemangiomas. As the child grows and becomes more active, a trauma to the lesion could become a very stressful event. Spontaneous bleeding from a lesion can also occur.
Another concern is that families may live in rural areas, that a direct and immediate access to a medical center is not feasible.
6. Psychological sequelae
One of the most important complications of a noticeable facial hemangioma is the affect on the psychological development. As children grow they develop a sense of self awareness after the age of one. This is also the time that they start sensing the feelings of others.
As the disfigurement of the child has an impact to the family members, the peers and many others, there may be a negative expressional feedback to the child. Soon the child will realize that there is something different on his/her face that makes other people stare at and commend negatively.
In early childhood, the presence of the lesion will affect the educational, social, emotional and intellectual development. These facts may lead to a low self esteem, isolation and a submissive personality.
As the affected child moves from the preschool to school age years, negative attitude from other children may be physiologically disturbing. The child is stigmatized and these stigmata of childhood years will follow the young patient throughout the course of his/her life. It is of paramount importance to treat early lesions causing a disfigurement, which may lead to psychological sequelae.
7. Skeletal distortion
The presence of a facial hemangioma will affect the facial skeleton. The bony structures of the face grow with the lesion. The pressure applied from the hemangioma to the underlying skeleton will affect the shape, the size and the normal outline of facial bones. A great degree of distortion may develop. The bony abnormality can be the expansion of the orbit, calvarial changes, flattening of the nasal pyramid, mandibular overgrowth, midface structural changes.
Cartilaginous destruction can also occur at the nasal alae and the pinna. It is important to realize that the bony distortion will magnify the disfigurement and further more it may require multiple complicated surgical procedures to be corrected. Early treatment of hemangiomas and prevention of skeletal distortion is very important.
8. High output cardiac failure
High-output heart failure is a condition that occurs when the cardiac output is higher than normal. There is a circulatory overload which may develop pulmonary edema, secondary to an elevated diastolic pressure in left ventricle. These patients have usually symptoms are of a heart failure. With time, this overload causes failure of the pumping activity of the heart. Cardiac output can be gradually reduced to low levels. This condition is usually seen with multiple cutaneous lesions, hepatic lesions or very large solitary hemangiomas.
This condition is a potentially lethal complication.
9. Disseminated intravascular coagulation
In this serious medical condition, the processes of coagulation and fibrinolysis are deregulated, and the result is widespread clotting with resultant bleeding. The triggering event of disseminated intravascular coagulation in cases of extended hemangiomas is a large blood clot in a rapidly growing lesion. Within this blood clot the platelets and other clotting factors are depleted.
Hemangioma treatment
Treatment
The timing of treatment is an important issue. There are no hard and fast rules and unfortunately, the timing is often dictated by the beliefs of the physician. It is important to realize that the early years of a child's life are the formative years of his/her psychological development. Clearly, disfigurement can adversely affect this. For this reason, we believe that early intervention is warranted. This must however be carefully weighed against the likelihood of complete involution (regression) of the hemangioma. Furthermore, the result of early intervention should leave a result that is as good as or better than the result of natural involution. This is clearly a difficult decision that should not be taken lightly. We advise the parents of the child to seek professional help and this should be given by several physicians. Unfortunately, this can be confusing since opinions will vary. Remember, these are only opinions, and nothing more.
Complications such as ulceration, congestive heart failure and failure to thrive clearly warrant early intervention. A hemangioma that interferes with a function such as speech or feeding should be treated early. The same applies to a hemangioma that could potentially block the child's airway.
There are several treatment modalities. Each has a role in the management of hemangiomas. The choice of modality should be determined by the lesion.
Systemic and locally injected steroids
The mechanism of steroids is unknown.
Steroids appear to affect the growth of hemangiomas and in some cases, can shrink the hemangioma. These drugs can be given systemically (by mouth) or they can be injected into the substance of the hemangioma (intra-lesional administration). In general, systemic steroids are more useful for the treatment of segmental hemangiomas and intra-lesional steroids are more useful for focal hemangiomas. The major advantage of intra-lesional injections is the reduction in systemic side effects.
Steroids have many side effects and for this reason, we prefer to limit the child's exposure to this potentially harmful drug. A child on steroids should be carefully monitored and although there are exceptions, we prefer to limit the child's exposure to three months of continuous steroid use.
One of the major disadvantages of steroid treatments is rebound growth. A high proportion of lesions will re-grow after treatment has been stopped. This usually prompts the physician to restart treatment and this can prolong the term of treatment. Another disadvantage is the rare but potentially dangerous side effect known as Addisonian crisis. Since our bodies make steroid which is necessary for certain important metabolic functions, the administration of a high dose, for a prolonged period (greater than 21 days), will stop the adrenal glands from manufacturing steroid. In times of stress these substances are essential for survival. When the child is exposed to stressful situations such as an infection, trauma or fever, the child will not produce these essential substances. For this reason, any child on steroids or any child who has been on steroids within the last six months should receive a stress dose.
Vincristine
Vincristine is a chemotherapeutic agent that has become popular especially for Kaposiform Hemangioendotheliomas and Hemangiomatosis with liver involvement. It is given through a central line weekly.
This drug has been part of several pediatric chemotherapeutic regimens and appears to have far fewer side effects than steroids. Its use was popularized recently for the treatment of children who were having difficulty weaning off steroids as well as for children whose hemangiomas were resistant to steroid treatment.
Propranolol
Propranolol is an antihypertensive drug that has been found to be active against hemangiomas. This is a recent finding that has caused much excitement in this field. The drug's effect appears to be active during both the proliferative phase (active growth) and the involution phase (regression). We have recently treated patients as late as two to two and a half years of age with Propranolol and we are surprised to see an effect.
The mechanism of action remains unknown and to date the only side effect documented appears to be a sudden drop in the blood glucose level of the child. This is usually seen when the child misses a meal. For this reason, we usually advise the parents to give the drug after a meal. If for some reason the child does not consume a sufficient quantity of food, the parents are then instructed to skip that dose. A make-up dose is not required. In this way, we have to prevent a drop in the blood glucose level.
We usually treat children with focal hemangiomas until about eight to nine months of age. This will hopefully prevent rebound growth. Children with segmental hemangiomas require a longer term of treatment due to the fact that segmental hemangiomas can proliferate for up to twenty-four months.
Pulsed Dye laser
Since the effective depth of penetration of a pulsed dye laser is minimal, laser is only appropriate for the superficial hemangiomas or the superficial component of a compound lesion. Early treatment is preferable, since we believe that early elimination of the hemangioma will allow collagen to regenerate and the skin texture will be more normal.
At some centers, a Nd:YAG laser is used to treat the surface as well as the deep component. In the right hands, this can be effective. However, the injudicious use of interstitial treatment with a Nd:YAG laser can result in significant complications. The standard of care for hemangiomas still remains a pulsed dye laser. Several other lasers are used from time to time but unfortunately these appear to carry a higher risk of scarring. While in experienced hands this may not be so, we typically do not recommend these other lasers.
Surgery
Surgical resection of hemangiomas is possible. It is important to realize that there is no text describing these procedures. The experience and past results of the surgeon are important.
Since hemangiomas are vascular tumors, the risk of severe blood loss is a possibility but in experienced hands, this risk is negligible.
Whether or not surgery is indicated will depend on a number of factors. In general, if there is a complication best treated with surgery or if it is likely that the outcome of spontaneous regression or medical management is not likely to leave a satisfactory outcome, then surgery should be considered.
The "wait and see" approach
The "wait and see" approach.
For many years in the past, the management of hemangiomas was directed towards the "benign neglect"policy. Observation of the lesion's clinical course was considered enough for this medical condition. The "wait and see" approach, had an obvious reason to be applied; "the hemangioma will eventually shrink, so what is the reason of treating a lesion that will disappear"?
Even today, a significant percentage of physicians, around the world, are still in favor of this approach. They suggest to "wait and see" and try to reassure the parents that, there is no reason for treatment.
We have to analyze this approach and try to determine if this 'benign neglect" can be applied safely.
One of the main reasons to support the 'do nothing" approach is the fact that the lesion will eventually disappear. This is the obvious argument in favor of this opinion.
There may have been other reasons, though.
Operating on a little patient with a vascular lesion requires specialized training, certain surgical skills and expertise. There is always the fear of extensive uncontrollable bleeding that may lead to hemorrhagic shock, if it is not controlled efficiently. Remember that the amount of blood loss, that a patient is able to tolerate, is proportional to the patient's weight. Babies have small weight and small blood volume, indeed!
Creating a scar, by excising a hemangioma of the face, could also be fearsome. When the extent of the scar is estimated preoperatively, there is always the fear that this will be a reminder of the lesion to the patient and the peers forever.
Utilizing other treatment modalities such as lasers or systemic and local medications also requires some experience. This experience was and to a certain extent still is limited, among otherwise very competent physicians, just because the treatment of hemangiomas was not widespread. So what is the right thing to do when having a patient with a hemangioma?
It is true that not at all cases are the same, nor the appropriate treatment is applied in the same manner. The physician has to recognize the reasons in order to decide to treat or not. The decision should not be based just on whether if he/she is capable of treating the lesion. It should be based on the indications for treatment. One of the main reasons for avoiding treatment was the fact that hemangiomas will eventually involute. Accumulating experience shows that, even when the lesion shrinks, there may be some elements left behind such as epidermal atrophy, scars from previous ulceration or residual telangiectasia. Studies have proved that 40% of the lesions involuting by the age of six and 80% of the lesions involuting by the age of twelve will require some form of corrective intervention.
It is of paramount importance to realize that a child with a prominent facial lesion at early childhood will most likely develop a psychological trauma. This fact is one of the most definite reasons to intervene early. Early intervention is defined as treatment before the development of self awareness (18-24 months), or if this is not possible, at least before entering into school environment. Children with a facial hemangioma will develop multiple emotional, educational, social and intellectual sequelae.
At this point we have to realize that the child is not able to take the decision for treatment on its own. It is the doctor with the parents that will take the decision for the child. This fact makes any decision even more difficult, because it will affect the child's life. This is one of the reasons why, in many cases, decision of not treating may not be the right one.
In many cases hemangiomas are associated with significant functional complications. Astigmatism and amblyopia from a periorbital lesion, skeletal distortion of the facial skeleton, airway obstruction, hemorrhage, high output cardiac failure, consumption of platelets and clotting factors, ulceration and epidermal atrophy, just to mention some.
All these factors are definite indications for treatment. It is not acceptable to approach, for example, a periorbital hemangioma with the 'wait and see approach'. The child will end up with visual impairment, which will most likely affect the rest of his/her life. It is also unjustified to "observe" the gradual skeletal distortion that will lead to bony developmental abnormalities, which will require extensive surgical corrections in the future.
The fear of an uncontrollable intraoperative bleeding played also a key role in the 'wait and see approach'. Many parents are still advised that the risk to benefit ratio of performing a surgical excision is not favorable. This opinion of course will make the parents decide against surgical treatment. The advances in surgical techniques, surgical expertise and training made the possibility of uncontrolled bleeding minimal. Surgical protocols upon the optimal way to surgically approach a hemangioma have been developed. Specialized training aims to provide the surgeon with all the necessary knowledge to safely perform the excision. With the aid of advanced technological instrumentation the specialist is able to operate and remove the hemangioma with minimal blood loss. The absence of intraoperative hemorrhage when patients are treated by well trained surgeons is an undoubtful fact.
Regarding the post operative surgical scar, the discussion should be focused on the unique healing characteristics of babies' skin. The skin elasticity and collagen fiber concentration is by far more prominent in little children. These facts have a favorable outcome when operating early on a baby's face. The resulting scar will be inconspicuous. The surgeon, is able to direct and "hide" the scar in certain natural lines of the face. Finally let's think that by removing a hemangioma, we "exchange" a disfiguring facial lesion, with a surgical scar which of course is by far less visible, having at the same time corrected the vascular anomaly.
For all these and many other individualized reasons, the old wait and see approach has to be reconsidered.
• Now days, vascular malformation clinics have been developed in many countries.
• The level of experience has considerably risen.
• The treatment modalities are, by far, improved.
• The advances of technology in lasers and surgical instrumentation were remarkable during the last few years.
• Propranolol has prevented many children from undergoing extensive surgeries.
• A lot of information is available through the internet.
• Many medical conferences are directed specifically in exchanging ideas and experience in this type of lesions.
• Many physicians work exclusively on this field.
• An enormous ongoing research is trying to reveal the pathogenesis of hemangiomas.
It is obvious that so many efforts are well under way, from all different aspects of the medical community, towards the quality of care for our little hemangioma patients.
• Why should we insist on doing nothing, when there are so many things to do?
• Who can deny a treatment option if this option exists?
• Who doesn't agree THAT EVERY CHILD DESERVES A NORMAL APPEARANCE?