Maxillofacial Trauma
Maxillofacial Trauma
Trauma is one of the most serious healthcare problems. It results in disfigurement, disability, or death. Although absolute numbers may be lately declining, it is the leading cause of death among teenagers and young adults.
Facial trauma is defined as any injury involving the hard and soft tissues of the face. It can present as an isolated injury or a fraction of the total injuries regarding a polytrauma patient. Motor vehicle accidents, interpersonal violence, self-inflicting wounds, sports injuries, burns, falls, work-related accidents, animal attacks, gunshots and blasts, are some of the causes related to facial trauma.
Facial injuries can vary from a simple bruising due to a mild hit, to a panfacial trauma. The mechanism, as well as the force of the injury, plays a key role in the severity of the wound.
Facial injuries are classified into two major categories:
1. Soft tissue injuries
- Contusions
- Abrasions
- Lacerations (simple, stellate, Flap-like)
- Avulsion
- Animal Bites
- Burns
- Cold injuries
- Nerve injuries
- Salivary gland injuries
2. Injuries to the facial skeleton
- Dentoalveolar injuries
- Mandibular fractures
- Trauma to the Temporomandibular joint region
- Fractures of the Zygomatic complex and arch
- Fractures of the Maxilla
- Le Fort I type fractures
- Le Fort II type fractures
- Le Fort III type fractures
- Nasal-Orbital-Ethmoid injuries
- Orbital Wall fractures
- Traumatic injuries to the Frontal Sinus
- Nasal fractures
- Combination of the above
Clinical presentation of facial injuries can vary considerably, depending on the facial structure involved. In cases of soft tissue trauma, the clinical signs are, most of the times, evident. The history given by the patient or the peers, combined with the visible result of the impact, make the diagnosis obvious.
In cases of skeletal injuries, clinical signs are depended on the fractured bone(s). Fractures of facial bones may be associated with pain, bruising, and swelling of the surrounding tissues although such symptoms can occur in the absence of fractures as well. Fractures of the nose, the base of the skull, or maxilla may be associated with profuse nosebleeds. Nasal fractures may be associated with deformity of the nose, as well as swelling and bruising. Deformity in the face, for example, a sunken cheekbone or teeth which do not align properly, suggests the presence of fractures. Asymmetry can suggest facial fractures or damage to nerves. People with mandibular fractures often have pain and difficulty in opening their mouths and may have numbness in the lip and chin. In cases of Le Fort fractures, the midface may move relative to the rest of the face or skull.
A thorough history regarding the nature of the event must be obtained. The physician will make a clinical evaluation regarding the overall physical condition as well as the relevant signs and symptoms. Radiographic examination is usually necessary to rule out or confirm the diagnosis, as well as for preoperative evaluation and treatment planning. Plain radiographs may be useful, but in most cases, a Computed Tomography of the head will be obtained.
Information regarding signs and symptoms, as well as the treatment options regarding different types of facial injuries, is provided below:
Injuries to the facial skeleton
DENTOALVEOLAR INJURIES
Dentoalveolar injuries refer to damage to the teeth, the gingiva, or the supporting structures. They can be isolated or associated with multisystem injuries. Among other general causative reasons, they may be encountered in the pediatric population as a result of child abuse.
Signs and symptoms include:
- Crown fracture
- Crown-root fracture
- Concussion to the tooth supporting structures
- Loosening (subluxation) of teeth
- Complete avulsion of teeth
- Comminution of the alveolar socket
- Fracture of the alveolar socket wall
- Fracture of the alveolar process
- Laceration of the gingiva or mucosa
- Contusion of the gingiva or mucosa
- Abrasion of the gingiva or mucosa
In most of the cases, injuries of the dentoalveolar complex are treated by our dental colleagues. Teeth restorations, teeth immobilization, root canals, resign splints, are done by general dentists, pediatric dentists, orthodontists, endodontists, prosthodontists, accordingly.
Frequently the patient will be initially seen by a maxillofacial surgeon, to rule out any additional skeletal injuries, or to repair intraoral lacerations. In cases of alveolar process fractures, in which the bone-teeth unit is displaced, the patient will have to undergo a reduction and splinting by the surgeon.
When dealing with isolated dental injuries, after the initial consultation with the surgeon, the patient will be referred to the appropriate dental specialists for further treatment.
MANDIBULAR (LOWER JAW) FRACTURES
A severe impact to the area of the lower face may result in a fractured lower jaw. Any part of the jaw may break, and the insult may be associated with dentoalveolar injuries as well. Except that, a lower jaw fracture may be associated with other facial fractures.
Signs and symptoms include:
- Change in bite
- Numbness of the lower lip
- Abnormal movement of the lower jaw
- Changes in facial contour
- Laceration and bruising
- Loose teeth
- Pain, swelling, redness
- Crepitation
In cases of a broken lower jaw, the patient’s general physical status must be carefully evaluated and monitored. The treatment is not performed as an emergency procedure. Any dental injuries must be treated at the same time if possible. Antibiotics are necessary in cases of compound fractures. The patient must receive pre and postoperative nutritional instructions. There are two ways of treating fractures of the lower jaw.
1. Closed reduction is a procedure during which the teeth are placed into the preoperative bite position. In this position, the upper and lower jaw are fixated with the use of bars and elastics placed around the teeth. This procedure is indicated: in cases of nondisplaced favorable fractures, in severely comminuted fractures, in cases of significant loss of overlying soft tissue, in most of the cases of an atrophic fractured lower jaw and in cases of children with developing dentition. In cases of an isolated lower jaw fracture, this procedure is usually done under sedation and doesn’t require hospitalization.
2. Open reduction and internal fixation is a procedure during which the surgeon gets direct access to the fracture site, the fracture is manually reduced, and fixation of the fractured segments is achieved with the use of plates and screws.
This type of treatment is indicated: in cases of unfavorable displaced fractures, in cases of multiple fractures of the facial bones, in some cases of lower jaw atrophy, in cases of delayed treatment where soft tissue is interposed between fragments and in some medical conditions in which mandibular movement is necessary. Many different surgical approaches can be utilized for an open approach. The surgeon can have access to lower jaw though incisions within the mouth or outside of the mouth. The choice is depended on the severity of the injury, the anatomical site, any coexisting trauma, the overall status of the patient, and the surgeon’s experience. In cases of an isolated lower jaw fracture, this procedure is usually done under general anesthesia and requires overnight hospital admission.
TRAUMA TO THE TEMPOROMANDIBULAR JOINT REGION
Trauma to the temporomandibular joint is anatomically included in the classification of lower jaw fractures. The complexity of the joint structure and its proximity to other important craniofacial structures makes the evaluation, diagnosis, and management particularly challenging. An experienced facial trauma surgeon must evaluate all cases of temporomandibular injuries.
Signs and symptoms include:
- Evidence of facial trauma
- Bleeding from the ear
- Swelling of the joint area
- Facial asymmetry
- Pain and tenderness in the joint area
- Changes of the bite
- A shift of the lower jaw midline
- Limited mouth opening
The main goal of treatment is the restoration of function.
Treatment options include:
1. Conservative treatment (observation and soft diet) is indicated in cases of nondisplaced fractures of the condyles in which a stable occlusion is seen, and no irregularities of the masticatory system’s function are noted. 2. Immobilization of the jaw followed by physiotherapy. This is the most common form of treatment. It is supported by the majority of the literature, and it is based on the principles of functional healing. A form of fixation of the jaws is necessary for a period that varies from few days to two weeks.
3. Open reduction and fixation are indicated in cases of displacement of the condyle into the middle cranial fossa, in cases where an adequate occlusion cannot be obtained with closed techniques and in lateral dislocation of the condyle, out of its capsule. Some other relative indications include cases of bilateral fractures in edentulous patients, when medical conditions prevent closed reduction procedures, or when bilateral fractures are associated with comminuted midfacial fractures.
Surgical access to the joint is mainly via incisions in front of the ear, below the lower jaw, or even through the mouth. When an open procedure is decided, the surgery is done under general anesthesia, and admission to the hospital will be required for the patient.
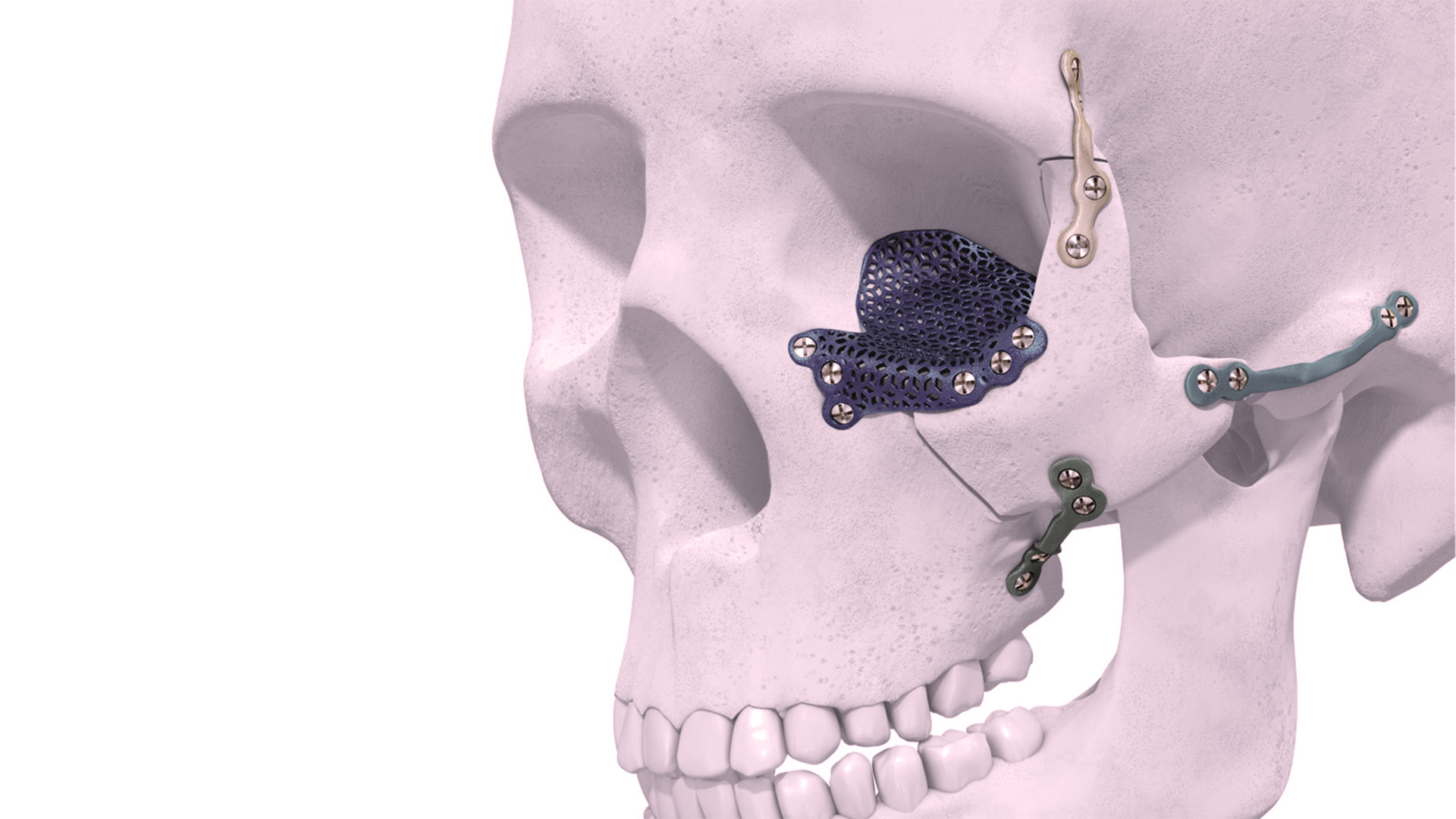
FRACTURES OF THE ZYGOMATIC COMPLEX AND ARCH.
The zygoma prominence within the facial skeleton makes it frequently exposed to traumatic insults. Usually, a zygomatic-complex fracture involves the bony wall under the eye socket, the zygomatic arch, the area where the lateral wall of the socket connects with the frontal bone and the zygomatic buttress.
Signs and symptoms include
- Swelling and bruising around the eye
- Flattening of the cheekbone
- Flattening over the zygomatic arch
- Pain
- Bruising inside the mouth (upper jaw sulcus)
- Limitation in mouth opening
- Numbness of the cheek, the side of the nose and the front upper teeth gums.
- A palpable gap on the lower bony margin of the eye socket
- Nosebleed
- Blood under the conjunctiva
- Crepitation
- Double vision
- Uneven projection of the eyeballs (lesser projection of the eye at the affected side).
The treatment usually requires an open reduction and internal fixation techniques. According to the type of injury, the bony displacement, the functional impairment, the aesthetic considerations and the overall condition of the patient, many different approaches are utilized. In cases of non displaced fractures, with no functional or aesthetic problems, just observation and a soft diet are necessary.
FRACTURES OF THE MAXILLA (UPPER JAW) AND LE FORT I, II, III TYPE FRACTURES
The upper jaw is one of the bones that form the bulk of the midface: It forms the roof of the mouth and houses the upper teeth, it forms part of the wall of the orbits, and the floor as well as the lateral wall of nasal fossa. Although isolated upper jaw fracture may result from certain assaults, usually the upper jaw is fractured following certain patterns, in which other facial bones may be involved. To further understand the types of injuries with a fractured upper jaw, we classify these injuries into the following three categories:
Le Fort I Fractures. These are caused by an anteroposteriorly delivered force, at a level above the upper teeth. This type of fracture involves floor of the nose, the lower third of the maxilla, the palate, and the pterygoid plates. The bone containing the upper teeth becomes separated as a horseshoe. The jaw is usually displaced posteriorly and inferiorly.
Signs and symptoms include:
- Open bite
- Swelling
- Pain
- Bruising
- Mobility of the upper jaw
- Nosebleed
- Sometimes numbness of the cheek
Le Fort II Fractures
The Le Fort type II fractures are caused by a superiorly directed force or an anteroposteriorly delivered force at the level of the floor of the eye sockets. The line of these fractures begins at the area of the junction of the nose to the frontal bone. It extends to the lateral wall of the maxilla ending at the back of the palate.
Signs and symptoms include:
- Swelling around both eyes
- Bruising around both eyes (raccoon eyes)
- Numbness of the cheek
- A palpable gap on the lower bony margin of the eye socket
- A palpable gap on the junction of the nose to the forehead
- Mobility of the upper jaw and the nose, as a unit
- Leak of brain fluid through the nose
- All other signs and symptoms of Le Fort I type
Le Fort III Fractures
In this very severe injury, the bony facial complex is separated from the cranial vault (craniofacial disjunction). It is usually caused by high-velocity impacts. The fracture line extends laterally across the nasofrontal junction, orbital walls and floor, zygomaticofrontal junction, zygoma, and pterygoid plate.
Signs and symptoms include:
- Dish face appearance
- Mobility of the nose-zygoma-upper jaw complex, together as a unit
- Leak of brain fluid through the nose
- Swelling and bruising around the eyes
- Generalized swelling of the face
- Increased distance between the medial corners of the eye fissures (telecanthus)
- All other signs and symptoms of Le Fort I and II types
In all of the above types of injuries, hospital admission is mandatory. The patient will be examined and evaluated by a team of different specialists. Neurological examination is very important as sometimes the magnitude of the applied forces and the mechanism of the impact may cause concomitant brain injuries as well. Management of brain damage is an absolute priority. After the initial examination, the patient is stabilized regarding airway, bleeding and circulatory issues. Definitive treatment of the facial fractures is initiated when the patient is able to sustain a lengthy procedure, the swelling is reduced, the neurological status is normal, and the treatment planning has been made.
Treatment of complex facial fractures of this kind requires extensive training and expertise. The surgical approaches and the mode of the surgeon’s actions are depended on the type of injury, the overall condition of the patient and the goals set for functional and esthetic restoration. Facial surgeons can perform open reduction and internal fixation of multiple facial bone fractures through hidden surgical approaches. In most cases, the surgeon will utilize either already existing lacerations due to the trauma, or other surgical approaches which will provide a very good esthetic appearance. The ultimate goal is to restore the function as well as to provide a good aesthetic appearance. Sometimes the initial treatment is followed by the necessary facial reconstructive procedures.
NASAL-ORBITAL-ETHMOID INJURIES (NOE FRACTURES)
Combined fractures of the nose, the eye socket walls and the ethmoids can occur from a direct blow at the area, or as a part of an excessive facial injury. The NOE complex consists of the nasal bones, frontal process of the maxilla, nasal process of the frontal bone, lacrimal bone, lamina papyracea, ethmoid bone, sphenoid bone and nasal septum. All these structures separate the nasal and orbital cavities from cranial cavity. The complex anatomy makes the management of NOE injuries particularly challenging. Half of these cases are associated with brain injury. The majority occurs as a result of a motor vehicle accident.
Signs and symptoms include:
- Fractured nose, often comminuted and displaced posteriorly
- Widening of the nasal bridge
- Nosebleed
- Swelling around the eyes
- Increased distance between the medial corners of the eye fissures (telecanthus)
- An overflow of tears onto the face (Epiphora)
- Bruising around the eyes
- Blood collection underneath the mucosa of the nasal septum
- Leak of brain fluid through the nose
- Forehead numbness
- Double vision
Treatment of Naso-Orbital-Ethmoid fractures should consist of careful evaluation and planning, along with detailed osseous reduction and fixation to achieve the best esthetic and functional restoration. Attention to the medial canthal tendons and proper repositioning if displaced is very important. Different surgical approaches have been described for the treatment of NOE fractures. These procedures will require a surgical team with experience in facial trauma surgery.
ORBITAL WALL FRACTURES
Orbital wall fractures can be divided into two parts. The anterior section refers to the orbital rim. The posterior section consists of the orbital roof, the orbital floor and the medial and lateral walls of the eye sockets. Fractures of the posterior section can occur by force directed inwardly or outwardly.
The term “blow out” fracture describes a fracture of the floor of the orbit (less frequently of the medial or lateral wall). This fracture is the result of a direct force applied to the globe. This trauma causes an increase in hydrostatic pressure within the eye socket, causing a deformation of the bony framework. We can identify isolated orbital wall “bow out” fractures, or fractures combined with a concomitant orbital rim fracture. In cases of orbital floor fractures, a displacement of the orbital contents to the maxillary sinus may occur, thus reducing the overall soft tissue volume of the orbit.
“Blow in” fracture is an inwardly displaced fracture of the orbital rim or wall resulting in decreased orbital volume. The inwardly displaced bone fragment acts as a space-occupying lesion and decreases intraorbital volume. This type of fracture is much less common. The presentation is typically associated with malar trauma that results in a depression of the maxillary sinus. This can result in an upward displacement of orbital floor contents, which causes superior displacement of the globe. This type of injury can be even more concerning than a blow-out fracture because it causes a decrease in orbital volume, which can lead to compression of orbital contents and subsequent ischemia or globe rupture from fracture fragments.
Signs and symptoms:
- Double vision
- Uneven projection of the eyeballs; lesser projection of the eye at the affected side-enophthalmos. (blow out fractures)
- Restriction of the eye movement due to entrapment of eye muscles
- Numbness of the cheek
- Uneven vertical position of the pupils (Vertical dystopia)
- Swelling of the soft tissues
- Bruising
- Bulging eye (blow in fractures)
In cases of “blow out” fractures, the main indication of treatment is nonresolving double vision within two weeks. To obtain better results, it is preferable not to postpone surgical intervention later. A large variety of materials including alloplastic, allogenic and autologous have been used to reconstruct the orbital floor fractures. The approach to the orbital floor can be either through an incision inside the lower eyelid or an external incision 2mm below the eyelashes.
Medial wall fractures may be treated following the same surgical indications and principles, like those applied for reconstruction of the orbital floor. Lateral wall fractures are rare.
In cases of a “blow in” fracture, no care is required for a minimally displaced fracture in the absence of functional problems. On the other hand in cases of a bulging eye, an optic nerve injury, a superior orbital fissure syndrome, or a globe rupture, immediate decompression and reconstruction are necessary.
TRAUMATIC INJURIES TO THE FRONTAL SINUS
Blunt trauma associated with motor vehicle accidents is the main causative factor of a forehead trauma. The frontal sinus is a cavity within the frontal bone. It has two tables one anteriorly which is palpable when we touch the forehead and one posterior which is the anterior margin of the cranial cavity. The frontal sinus drains into the nose. The proximity of the frontal sinus to the brain makes any untreated condition potentially serious. Complications of a frontal sinus fracture may appear years after injury.
Signs and symptoms:
- Forehead soft tissue swelling of the
- Smell sense alterations
- Leakage of cerebrospinal fluid
- Depression of the forehead contour
- Forehead lacerations
- Forehead pain
- Forehead numbness
The best way to evaluate a posterior wall fracture is to obtain a Computed Tomography.
Treatment of frontal sinus (FS) fractures can be complex. A great degree of controversy exists regarding accepted protocols of treatment. The surgeon should have a clear algorithm in mind for the management of different types of frontal sinus fractures.
Treatment options include observation, open reduction and internal fixation, sinus obliteration, and sinus cranialization. In cases of linear anterior table fractures observation is recommended, provided that the drainage system to the nose remains intact.
When the anterior fractured table is displaced, the surgeon may choose to elevate and fixate the segments, or proceed to the obliteration of the sinus (meticulously debride all mucosa from the sinus and fill the sinus cavity with autologous fat).
In cases of nondisplaced posterior table fractures, a lot of controversies exist regarding their treatment between conservative and more aggressive approaches. If the posterior table is displaced, the choice of treatment is between obliteration and cranialization (removal of the posterior table to allow the brain to expand into the frontal sinus).
Fractures of the forehead do not require immediate surgical intervention unless there is a neurosurgical or ophthalmologic emergency. The need for long-term follow-up of patients with frontal sinus fractures is very important. The risk of mucocele formation or other late complications is significant.
NASAL FRACTURES
The nose's protruding position coupled with its relative lack of support predisposes it to fractures. Nasal fractures represent the third most commonly broken bone in the body, and the nose is the most commonly broken facial bone. When a nasal fracture is left untreated or is underestimated, significant long-term functional and cosmetic problems may result. Treatment of long-term complications after a major injury is difficult. Prompt appropriate treatment prevents functional and cosmetic changes.
Signs and symptoms:
- Laceration
- Bruising
- Hematoma of the septum
- Mucosal tears
- Nosebleed
- Difficulty in breathing
- Palpation of a bony step
- Swelling of the eyelids
- Subconjunctival hemorrhage (blood under the membrane that covers the eyeball)
- Pseudotelecanthus. (increased distance between the eye corners due to swelling)
Reduction of a nasal fracture is indicated in patients with a significant cosmetic deformity or functional compromise. The preferred time for intervention is within the first few hours following the accident. This will give to the surgeon an opportunity to manipulate the fragments easily, as well as to have a very good idea about the success of the reduction, because facial tissue distortion, due to the developing swelling, is not yet peaked. When this time window has passed, it is better to intervene after the swelling has subsided, usually after 3-7 days. Many cases of nasal fracture do not require treatment when the fragments are not displaced, and there is no visible change of facial appearance.Two surgical options are implemented for the treatment of nasal fractures:
The closed reduction is used for unilateral or bilateral fractures of the nasal bones or fracture of the nasal septal complex that is deviated less than one half of the width of the nasal bridge.
Most patients who treated with closed reduction undergo the procedure in the clinic and may be discharged home following the procedure.
The open reduction is indicated for extensive fractures, in cases of deviation of the nasal pyramid greater than one half of the width of the nasal bridge, in a displaced fracture of the caudal septum or an open septal fracture, and if a deformity is still observed after all efforts of a closed reduction are exhausted. Patients, who require an open reduction, undergo the procedure under sedation or general anesthesia at the hospital. Usually, they are discharged the same day.
Soft tissue injuries
CONTUSIONS
The medical term “contusion” refers to the more commonly used word “bruise.” A bruise of the facial soft tissues involves damage to the capillaries under the skin. Blunt trauma may crush these very small vessels, and blood may leak out. The result will be swelling and bruise in the affected area. Sometimes a laceration is also evident. A bruise can be seen immediately after the blow or may take hours to become visible. The color of the skin may be purple or dark blue and may change during healing to a fading brown, green or yellow. Pain and tenderness are frequently associated with a facial contusion.
Facial bruises may present as an isolated injury or may be a clinical sign of a more complicated situation, such as a coexisting broken bone.
When should a patient seek medical advice?
- When you experience nausea or vomiting after the blow
- When you have a persistent headache
- If you lost consciousness after the trauma
- In cases of being confused
- If you see a lump growing fast (possible hematoma)
- If you experience changes in vision
- If you see blood in the whites of your eye
- If you have a nosebleed
- If you’re experiencing a lot of pain
You should also consult a physician if you get bruised very easily or without an obvious reason, as these can be a clinical sign of an underlying blood coagulation abnormality.
Treatment of a facial bruise involves the application of ice packs, and your physician may prescribe some painkillers and anti-inflammatory medications. The swelling may take up to a week to subside, but the discoloration can take longer.
ABRASIONS
An abrasion or a “brush burn” results from deflecting type trauma, when the skin is rubbed off. It is a minor injury that may occur quite frequently in many ordinary events. The upper layer of the skin is scraped off and leave a raw, bleeding undersurface. Although most injuries of this type involve the extremities, facial injuries are not uncommon. Falls, sliding along the ground, some sports, etc. may be the cause. Small particles of dirt, grease, and other pigments may be embedded in the exposed surface, and if become fixated, a traumatic tattoo may be formed. Most abrasions can be treated at home, and a trip to the emergency room is typically not necessary.
Signs and symptoms include bleeding, discomfort due to the exposure of nerve endings, and visible alteration of the skin’s architecture since the upper layer is peeled off.
When should a patient seek medical advice?
- For a large abrasion of the face
- When the abrasion is located close to your eyes
- If the wound is deep and you can see fat or muscle
- If you cannot clean the area from the dirt
- If you think that a foreign object is lodged in the wound
- If you had an injury caused by a dirty or rusty object
- In cases of an animal or human bites
- If your last tetanus vaccination was more than five years ago
Treatment is directed towards copious irrigation of the affected area to remove dirt and other pigments. The abrasion should be covered with a thin layer of an antibiotic ointment and dressed with gauze. Healing is expected in 7-10 days without significant aesthetic issues if only the superficial layer was scraped off. The patient should avoid direct exposure to sunlight for at least six months after the injury. A sun blocking agent is recommended.
If the affected area continues to be warm, swollen, or red, or there is a discharge from the wound, an infection may be present, and antibiotic treatment may be necessary.
LACERATIONS
Lacerations may be caused by a sharp, penetrating object or can be the result of a crushing type of injury. The continuity of the skin structure is disrupted, and a scar will be the result of any facial laceration. As all patients are especially concerned about scars on their face, it is important to seek proper medical advice early, so that the least noticeable scar will remain. Due to their cosmetic importance, a detailed and meticulous approach to their evaluation and treatment is necessary.
The physician will evaluate the nature of the traumatic force; any symptoms of a possibly associated head injury, the time elapsed since your injury, signs of wound contamination and the presence of foreign bodies. Your doctor will also consider the location of the involved facial zone, the length of laceration, the depth of laceration (epidermis, dermis, subcutaneous fat, muscle, or bone), the shape of laceration (linear, curvilinear, stellate, or corner) and if skin loss exists.
We can classify facial lacerations in three groups: simple lacerations, stellate lacerations, and flap-like lacerations.
The treatment involves meticulous wound debridement, removal of any necrotic tissue and closure of the wound with sutures. The preferred method of treatment is primary closure at the time of presentation. The delayed primary closure is warranted for wounds with signs of infection, swelling, hematoma or in cases of delayed presentation in which the possibility of infection is increased.
What exactly is a stitch? A stitch is a piece of thread that is used to sew the skin of a wound together. Stitching is a way surgeons can close certain types of cuts. The doctor will pass a special threaded needle through the edges of the wound and tie knots to hold the stitches in place.
Do I need stitches? If your cut is long, deep, or wide, you may need to ask for medical assistance. A wound that is left to heal on its own may leave a noticeable scar, may get infected or may take longer to heal. Scrapes and minor cuts, on the other hand, may not require stitches. In any case, all facial wounds should be evaluated by a physician.
Is it painful? The doctor will give you some numbing medicine before cleaning and stitching the wound. No pain is anticipated during the procedure.
What should I do after the procedure? Your doctor will give some instructions to you that are important to follow. Initially, you must keep the wound dry and covered with a bandage. Once keeping the wound covered is no longer necessary, you can gently wash them as a part of your regular hygiene, but you should avoid getting your stitches too wet. After the area is washed, you must keep it dry and put an antibiotic ointment on it. You must avoid any activity that may interfere with the wounded area, making sure that you always keep the stitches intact.
When should I be worried? You should call the office if the stitches break or see that the wound opens up again, if you notice that the area is red or swollen, if you see pus draining from the wound or your temperature level rises.
When will my stitches be removed? You will be instructed by your doctor when to come back for suture removal. Usually, stitches on the face will be removed within 5-6 days after their placement.
Is there something I should do after suture removal? You should avoid direct sunlight exposure and protect the scar from the sun. Use sunscreen on the area or wear a hat that protects the scar. You may be instructed to apply some ointments to improve the healing process further.
AVULSIONS
Traumatic facial avulsion is an injury in which the skin is forcibly detached from its position. The incidence of actual loss of skin is rare. In most cases, in which initial evaluation may suggest missing tissue, usually detailed examination reveals parts of the “absent” tissue rolled under the wound edges. In cases of small defects, the surgeon will be able to approximate the edges of the wound by undermining the adjacent skin. In cases of larger defects, some form of reconstructive procedures will have to be utilized. Free skin grafts and local or regional flaps can provide one stage repair of avulsion defects. In very large degloving defects, careful evaluation and staging of the treatment sequence are necessary.
ANIMAL BITES
Animal bites are not rare. Records in the US has shown that up to 1% of the emergency room visits annually were related to a dog or a cat bite. Dog bites are by far more common of the reported animal bites. The facial region is involved mostly in younger age groups.
A physician must evaluate all animal bites. The concern is not just the esthetic outcome. The contagious microbial load is a major issue in every case of an animal bite. Rabies is also a serious consideration.
The surgeon will evaluate the wound under local or general anesthesia depending on its extent.
Copious irrigation and debridement are required. Adequate control of bleeding must be achieved. Debris, dried clots and necrotic tissue must be removed. In most cases, laceration type wounds can be closed primarily, whereas puncture type wounds must be left open and will require a delayed closure. Techniques such as skin grafts or regional flaps may be utilized accordingly.
The patient will receive antibiotics for prevention or treatment of associated infections that may be caused by the bite. Rabies prophylaxis is recommended for suspected animals or when the incident occurred in areas that the incidence of rabies is high. Tetanus prophylaxis is considered as well.
Human bites are also evaluated and treated under the same principles as with animal bite cases.
BURNS
Facial burns can result from thermal, chemical, electric and radiation insults. They can vary from minor local skin damages to severe debilitating injuries. The head and neck region is frequently involved.
High voltage electrical burns destroy the underline tissues extensively, as compared to the skin. Low voltage damage, on the other hand, may not be destructive. Chemical injuries cause damage for as long as they are in contact with the skin. Alkali burns are more serious compared to acid burns, as they penetrate deeper into the skin layers and cause progressive damage for hours after the initial contact. Radiation burns’ severity is related to the time of exposure, the wavelength characteristics and the type of the patient’s skin. Heat (flame, hot steam) burns are the most common types of facial burns and can be very destructive.
When the patient presents with a minor injury and the history of the insult is clear, then treatment can be undertaken in an office-based setting. Patients with severe burns are initially managed in a specialized burn unit.
Criteria for hospital admission are:
- Infants
- Young children with burns > 10% of their body surface
- Older children and adults with burns > 15% of their body surface
- Elderly patients
- Suspected child abuse or crime
- Chemical injuries with suspected underlying destruction
- Swelling of the eyelids resulting in obstruction of vision
- High voltage injuries
- Upper respiratory tract complications
- Medically compromised patients
Surgical treatment is directed to the restoration of function, comfort, and appearance. The goal of the reconstructive surgeon is to minimize the residual deformity by restoring the patient to a near-normal appearance. Functional restoration is also crucial. Treatment sequence includes the initial assessment and stabilization, early care of the burn wounds, late care of the burn wounds, followed by reconstructive procedures accordingly. Long-term psychological support must be provided in cases of devastating effects on appearance and residual functional impairment.
COLD INJURIES
Cold injury is described as a part of all possible facial insults. Although rare in a Mediterranean climate, it deserves to be mentioned as some patients may be exposed to contributing weather conditions. Cold exposure may result in a variety of injuries due to the human body's difficulty to compensate for low temperatures
Homeless people, psychiatric patients, military personnel, elderly patients could be at risk under certain circumstances. Other groups of higher risk may include patients with peripheral neuropathies or peripheral vascular disease. In general, we can identify two forms of cold injuries; cases in which a body part(s) is affected (peripheral injury) and cases in which the entire body is affected (hypothermia). Many times a combination of both conditions is evident.
The peripheral cold injuries may be evident in a clinical spectrum of varying severity. Facial cold injuries usually affect the nose, the ears, and the cheeks. The most common cold injuries of the facial tissues are:
- Frostnip It is a mild form of a peripheral cold injury, usually involving the nose and the ears. It occurs when being in very cold air without adequate protection. Treatment involves warming of the exposed area.
- Chilblain It is a more severe form characterized by the presence of red lesions or blisters, erosions, even ulcers. It usually manifests in hands and feet as well as on the face. The lesions will most likely resolve in 10-20 days although a recurrence may be seen when the affected part is exposed to low temperatures again. Treatment involves warming, massaging as well as the application of a lubricant.
- Frostbite It is a severe form of tissue injury from exposure to low temperature. Clinical signs include hyperemia and edema, large blisters and bullae, vesicles filled with reddish fluid and tissue necrosis.
In cases of only skin and subcutaneous tissue involvement, the skin is cold, pale to white, and nonblanching. Sensation usually is lost, whereas pain may be initially apparent in the affected area. Swelling will increase gradually. In more severe cases in which deeper tissues are involved, the affected area is hard, woodlike, without sensation. It may have a gray color or can be cyanotic and most likely will not respond well after rewarming.
Treatment in cases of facial involvement follows the protocols of frostbite care, as in any other part of the body.
Attention must be directed to identify and control systemic hypothermia first.
Gradual rewarming of the affected site is necessary.
After rewarming, the skin is washed gently to remove any residual dirt or pigments.
The skin is then carefully dried.
Tetanus prophylaxis is indicated with a tetanus vaccine. Antibiotics are necessary only when signs of infection are present. Ibuprophen is given systemically, and Aloe Vera is applied topically.
The blisters containing clear fluid are debrided in contrast to the blisters filled with hemorrhagic fluid that are left intact to rupture.
As it is difficult to estimate the depth and the extent of tissue destruction surgical debridement is delayed unless infection develops.
The damaged tissue should be allowed to demarcate.
If necrosis or permanent tissue damage occurs a thorough treatment planning, tailored to the specific condition, should be done.
Reconstructive facial surgery can provide solutions in cases of tissue loss.